UVC EFFICACY
Published efficacy for UVC germicidal dates back as early as 1876. The effectiveness of UVC has been well documented in medical environments, driven by the critical need for effective and efficient solutions to combat widespread multi-drug resistant and healthcare acquired infections (HAI).
With the advent of COVID-19, the general population now requires immediate protection against a deadly virus. Patriot UVClean devices are designed on more than a century of lessons learned and established successes. Our appliances serve not only the medical industry, but also deliver a proven answer for safety in schools, hotels, churches, government buildings, merchants, and public environments.
The following information addresses UVC efficacy for the purpose of air and surface disinfection.
Historical Milestones
| 1845 | Scientists learn that microorganisms respond to light. |
| 1877 | Downes and Blunt observed that exposing test tubes containing Pasteur’s solution to sunlight prevented the growth of microorganisms inside the tube and, upon increased exposure durations, the test tubes remained bacteria-free for several months. |
| 1878 -1903 | Several breakthroughs by Downes, Blunt, Duclaux, Koch, Geisler, Ward, and others show that the ability of light to inactivate microorganisms is dependent on the dose (intensity X time) and wavelength of radiation with continuous refining of the sensitivity of the specific typed of microorganism. |
| 1903 | Nobel Prize for Medicine is awarded to Neils Finsen for his use of UVC against lupus vulgaris and tuberculosis. |
| 1933 | Gates publishes the first analytical bactericidal action spectrum with peak effectiveness at 265nm very near to the 254 nm output of low-pressure Hg germicidal lamps. |
| 1933 | Wells presents the concept of airborne infection via “droplet nuclei” evaporated droplets containing infectious organism that can remain suspended in the air for extended duration. |
| 1935 | Wells and Fair demonstrate the ability of UVGI to efficiently inactivate airborne microorganisms and prove the concept of infection via the airborne route. |
| 1937 | Wells et al. use upper-room UVGI to prevent the epidemic spread of measles in suburban Philadelphia day schools where infection outside the school is unlikely. |
| 1956-1965 | Riley exposes guinea pigs to originating from an occupied TB ward and proves that TB is spread via the airborne route. A group of guinea pigs receiving the infected air via a UVGI irradiated duct were not infected, while a group receiving air via a non-irradiated duct were infected. |
| 1969-1975 | Riley et al continue UVGI evaluations, show reduction of concentrated aerosolized test organisms , determine virulent tubercle bacilli and BGC to be equally susceptible to UVGI, and demonstrate disappearance rate of aerosolized of BGC. |
| 1985 – 1992 | After decades of decline, unexpected resurgence in TB in the US ignite renewed interest in UVC. |
| 1992– 2000s | New in-depth efforts undertaken, aimed toward quantitatively examining UVC efficacy, safety, and proper use in medical use cases. |
| 2009 | Escombe et al significantly reduce TB transmission to guinea pigs housed atop an occupied HIV-TB ward, providing first controlled clinical evaluation. |
| 2010 – 2015 | Interest escalates due to multi- and extensive drug-resistant TB, bioterrorism, influenza pandemics, SARs, MERs, |
| 2016 – 2018 | Over 20 microbicidal studies and 12 Hospital Acquired Infection (HAI) reduction studies prove effectiveness and recommend UVC. |
| 2019 – 2020 | COVID-19 pandemic escalates interest in UVC; CDC, NIOSH, and others recommend and endorse UVC for disinfection and mitigation against the COVID-19. |
Studies and Testing
Medical Field Use Cases
A comparison of the efficacy of multiple ultraviolet light room decontamination devices in a radiology procedure room
Cadnum, Annette L. Jencson, Gestrich, Livingston, Karaman , Benner, Wilson, Donskey
https://doi.org/10.1017/ice.2018.296 | January 2019
Vertical tower low-pressure mercury devices, compared, achieved 2 log10CFU or greater reductions in VRE and MRSA and ~1 log10CFU reductions in C. difficile spores. Conclusion stated many currently available UV devices could provide an effective and efficient adjunct to manual cleaning and disinfection in radiology procedure rooms.
Impact of Ultraviolet Germicidal Irradiation for No-Touch Terminal Room Disinfection on Clostridium difficile Infection Incidence Among Hematology-Oncology Patients
David A. Pegues, Jennifer Han, Cheryl Gilmar, Brooke McDonnell, and Steven Gaynes
https://doi.org/10.1017/ice.2016.222 | October 2016
During a 52-week intervention period, UVGI was deployed for 542 of 2,569 of all patient discharges (21.1%) on the 3 study units. The CDI rate declined 25% on study units and increased 16% on non-study units during the intervention compared to the baseline period. Results detected a significant association between UVGI and decrease in CDI incidence (incidence rate ratio [IRR], 0.49; 95% confidence interval [CI], 0.26–0.94; P=.03) on the study units but not on the non-study units. The study concluded that targeted deployment of UVGI to rooms of high-risk patients at discharge resulted in a substantial reduction of CDI incidence without adversely impacting room turnaround.
Room Decontamination with UV Radiation
William A. Rutala, Maria F. Gergen, David J. Weber
https://doi.org/10.1086/656244 | Jan 2015
The effectiveness of UV-C radiation in reducing the counts of vegetative bacteria on surfaces was more than 99.9% within 15 minutes, and the reduction in C. difficile spores was 99.8% within 50 minutes. In rooms occupied by patients with MRSA, UV-C irradiation of approximately 15 minutes duration resulted in a decrease in total CFUs per plate.
Disinfectants used for environmental disinfection and new room decontamination technology
William A. Rutala, Maria F. Gergen, David J. Weber
https://doi.org/10.1016/j.ajic.2012.11.006 | May 2013
UVC advantage comments include its ability to achieve substantial reductions in vegetative bacteria, whereas cleaning has been demonstrated to be sub-optimal because many environmental surfaces are not cleaned as well as its ability to substantially reduce C difficile spores as low-level disinfectants have only limited or no measurable activity against spore-forming bacteria. UVC system is residual free, and they decontaminate all exposed surfaces and equipment in the room. The study notes that compared to Hydrogen Peroxide Vapor system (another popular ‘no-touch decontamination” system), the UVC system offers faster decontamination, which reduces the “down” time of the room before another patient can be admitted. And noted that a UV reflective wall coating reduced the time necessary to decontaminate a room using a UV-C emitting device from 25 minutes to 5 minutes for MRSA and from 44 minutes to 9 minutes for C difficile spores.
Portable UVC Devices Use Cases
The effectiveness of germicidal wipes and ultraviolet irradiation in reducing bacterial loads on electronic tablet devices used to obtain patient information in orthopedic clinics: evaluation of tablet cleaning methods
E.M. Allen, M.F. McTague, C.P. Bay, J.G. Esposito, A. von Keudell, M.J. Weaver https://doi.org/10.1016/j.jhin.2020.04.014 | April 2020
This study evaluated targeted irradiation of a small object. Using UV irradiation between each patient encounter led to significantly lower bacterial contamination rates (RR = 0.29 (95% confidence interval (CI) = 0.09–0.95)) compared with no routine cleaning.
Decontamination and Reuse of Filtering Face-piece Respirators
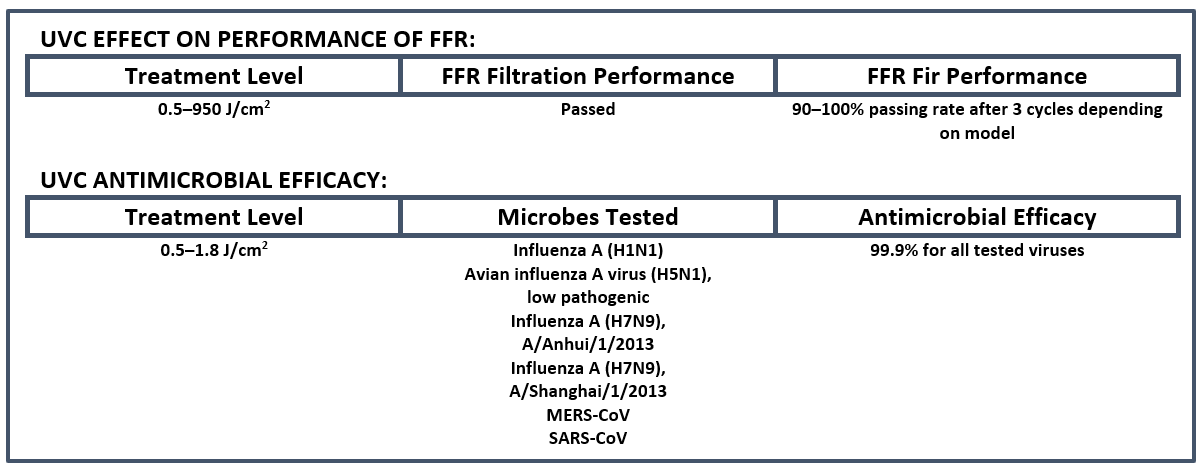
Acceptable filtration performance was recorded for eleven FFR models exposed to various UV doses ranging from roughly 0.5–950 J/cm2 and UVGI was shown to have minimal effect on fit. CDC published test results shown in the following table:
School Use Cases
The Environmental Control of Epidemic Contagion. I. An Epidemiologic Study of Radiant Disinfection of Air in Day Schools.
WF Wells, MW Wells, TS Wilder –
American Journal of Hygiene, 1942
The object of this investigation was to study the effect of irradiating the air of classrooms and ” home rooms ” in schools on the epidemic spread of droplet infections. Two schools were used. The Germantown Friends School and the Swarthmore public schools. In both cases the primary departments used the irradiated rooms, those occupied by the higher classes were not treated. Results of the 1941 measles epidemics at Germantown and Swarthmore reported rates among the primary irradiated classes, 14.5 per cent at Germantown, 15.7 per cent at College Avenue, 9.0 per cent at Rutgers Avenue drastically different to the upper unirradiated classes, 55.3 per cent at Germantown, 51.8 percent at Swarthmore. Patterns of the epidemics in the two schools were strikingly different from any previous experience.
Community-Wide Use Cases
Ventilation in the Flow of Measles and Chickenpox through a Community. Progress Report, Jan. 1, 1946, to June 15, 1949, Airborne Infection Study, Westchester County Department of Health.
Wells, Mildred W. ; Holla, W. A.
Journal of the American Medical Association 1950 Vol.142 No.17 pp.1337-44
Three- and half-year study directed towards finding the channels of flow of measles and chickenpox infection through a suburban community near New York. The spread of infection in two villages presented a contrast. In one the infection was protected from dynamic spread by the use of ultraviolet light, but this was to some extent counteracted by the frequent introduction of infection from surrounding villages. In the other, dynamic spread occurred within the village, but the latter was protected from frequent re-introductions of infection from without, by the ultra-violet irradiation methods adopted in the neighboring village.
Endorsements Specific to Use for COVID-19
Implementing Filtering Facepiece Respirator (FFR) Reuse, Including Reuse after Decontamination, When There Are Known Shortages of N95 Respirators
https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
An effective FFR decontamination method should reduce the pathogen burden, not harm the fit or filtration performance of the FFR and should present no residual chemical hazard. NIOSH reviewed the literature on decontaminating FFRs because of these considerations. NIOSH found that, as of April 2020, ultraviolet germicidal irradiation, vaporous hydrogen peroxide, and moist heat have shown the most promise as potential methods to decontaminate FFRs.
Guidelines for Environmental Infection Control in Health-Care Facilities
Recommendations of CDC & Healthcare Infection Control Practices Advisory Committee (HICPAC)
https://www.cdc.gov/infectioncontrol/guidelines/environmental/index.html
“Ultraviolet germicidal irradiation (UVGI) is effective in reducing the transmission of airborne bacterial and viral infections in hospitals, military housing, and classrooms…”.
Operating Schools During COVID-19: CDC’s Considerations
https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools.html
“Maintaining healthy environments: Consider using ultraviolet germicidal irradiation (UVGI) as a supplement to help inactivate SARS-CoV-2, especially if options for increasing room ventilation are limited.”
Illuminating Engineering Society (IES) Photobiology Committee Report Germicidal Ultraviolet
https://www1.fsgi.com/wp-content/uploads/IES-CR-2-20-V1-6d.pdf |April 2020
IES research states that ultraviolet C germicidal can effectively inactivate the virus which is responsible for COVID-19 provided the virus is directly illuminated by UVC at the effective dose level. UVC can play an effective role with other methods of disinfection.
Recommended Resources: UVC Efficacy & Endorsements
Kowalski W (2009). Ultraviolet Germicidal Irradiation Handbook, UVGI for Air and Surface Disinfection, Springer-Verlag, Berlin.
CDC Guidelines for Environmental Infection Control in Health-Care Facilities. 2003 (Updated July 2019)

UVClean Sterilizer™ 120w
UVClean Mini Sterilizer™

UVClean Wand Sterilizer™


